Pain causing insomnia? Put it to Rest
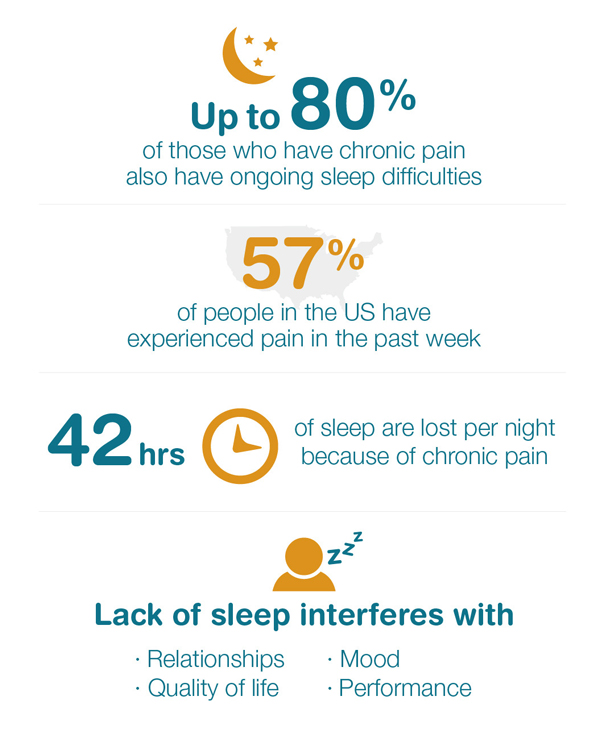
More than half the US population faced physical pain in the past week. Up to 80 percent of those people also face ongoing sleep problems.
This isn’t a coincidence—pain and sleep issues often impact each other, resulting in a vicious cycle of sleep loss and increasing pain symptoms.1 But it doesn’t have to be this way. Sleep therapies and medications can help those with pain get more shut-eye, which can improve the sensation of pain as well as mood, energy and performance.
How are Pain and Sleep Related?
Bedtime routines generally include eliminating all distractions to relax and fall asleep—like quieting the room and turning off lights and electronics. However, after quieting your environment, the only thing left for your brain to focus on is the pain, which only increases the perception of pain. Because of this, people who have chronic pain often have trouble falling asleep, get less deep sleep and wake up more often throughout the night. This results in less refreshing, poorer quality of sleep.2
However, if you’re facing a sleep disorder or aren’t following a sufficient sleep routine, your sleep deprivation can lower your pain threshold, worsening your existing pain.3
The link between pain and sleep varies from person to person. The first step is to figure out which is the root cause of the other.
What are Ways to Help Get Sleep or Reduce Pain?
Improving sleep with medication isn’t always the preferred route, since people who have chronic pain such as arthritis, fibromyalgia or diabetic nerve pain are also likely taking other medications to curb their pain symptoms. Additional sleep medications may interfere with their current pain medicines.
Before starting sleep therapies, investigate your bedtime routine. Sleep specialists often suggest these standard guidelines for good sleep hygiene:4
- Use your bed for sleep and sex only. Avoid sleep-inhibiting behaviors in your bed, such as reading, watching TV or worrying.
- Go to bed only when you’re tired. If you’re unable to fall asleep within 15-20 minutes of getting in bed, get up and go into another room and find a relaxing activity. Return to bed only when sleepy again.
- Follow a sleep schedule. Maintain a regular wake time regardless of the amount of sleep that night. Avoid naps during the day.
- Watch what you eat. Stay away from too much caffeine and alcohol. Monitor how late you eat.
- Exercise—but not within a couple hours of bedtime.
If you’re still struggling with pain-related sleep problems after reviewing your sleep hygiene, some specialists recommend cognitive behavioral therapy for insomnia (CBT-I). This type of therapy is designed to help people change the negative thoughts and behaviors that keep them from sleeping often preferred over medication because it has no side effects.
Another sleep therapy strategy is muscle relaxation therapy. Through progressive muscle relaxation (first tensing them up then releasing) and guided meditation, this technique helps calm pain and distract from restless thoughts.
Any kind of relaxation therapy involves guidance from a professional over a period of sessions.
If you have chronic pain and trouble sleeping, talk to your doctor to see what treatment options would be recommended.
Sources:
1 Cleveland Clinic
https://health.clevelandclinic.org/2015/12/managing-insomnia-for-those-with-chronic-pain/
2 Spine Health
http://www.spine-health.com/wellness/sleep/chronic-pain-and-insomnia-breaking-cycle
3 WebMD
http://www.webmd.com/sleep-disorders/features/pain-sleep#1
4 National Sleep Foundation
https://sleepfoundation.org/sleep-disorders-problems/pain-and-sleep/page/0/1


